
Lyrica With Suboxone: Risks And Safe Practices
The Recovery Team-Newton explores whether taking Lyrica with Suboxone is safe. Explore potential risks and guidelines
Depersonalization disorder is characterized by persistent or recurring feelings of detachment from one’s self. People with DPD often describe these experiences as feeling like they are living in a dream or movie, where their actions and thoughts seem disconnected from their control.
Understanding depersonalization disorder in the context of drug use is important for identifying the issue and seeking appropriate help. This guide explores how drug use can be a potential trigger for DPD and highlights the types of drugs and how they affect the brain to cause these symptoms.
Drug-induced depersonalization affects a significant portion of individuals who use substances recreationally or for medical reasons. Here’s what the article entails:
Contact The Recovery Team-Newton at (508) 978-2772 for information on different treatment options designed to support you in mental health recovery.
Depersonalization disorder (DPD), also known as depersonalization-derealization disorder (DPDR), is a mental disorder where a person feels disconnected from their own body and thoughts. This experience can be distressing and make it hard to connect with reality.
The exact cause of depersonalization disorder is not well understood, but it can be triggered by severe stress, trauma, or substance abuse. Drugs like marijuana, hallucinogens, and dissociative agents can alter the brain’s processing of self-perception, leading to derealization symptoms.
It is sometimes associated with other mental health issues such as anxiety, depression, or post-traumatic stress disorder (PTSD). Some studies indicate that it may be a way for the brain to cope with significant distress.
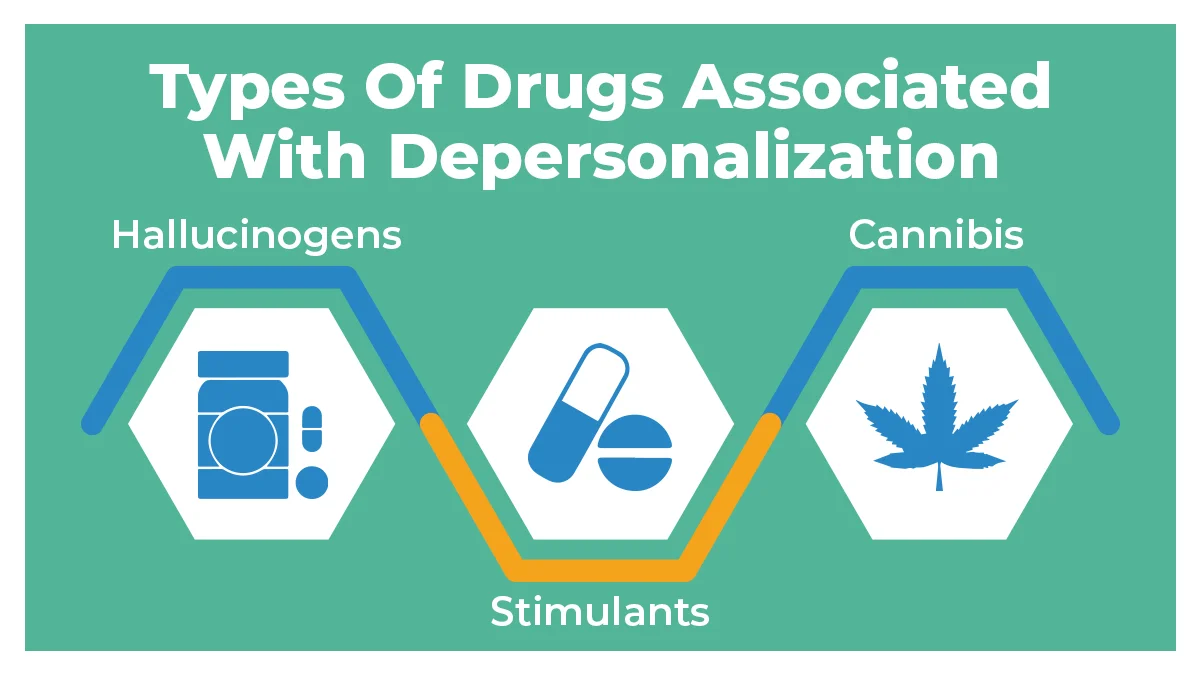
The effects of drugs on perception and cognition can sometimes lead individuals to experience depersonalization. Some common drug types may include:
Hallucinogens, such as LSD, psilocybin mushrooms, and MDMA, can induce feelings of depersonalization by altering perception and cognition. These drugs can create strong sensory experiences, leading to a distorted sense of self and reality.
Stimulants like cocaine, amphetamines, and methamphetamine can also trigger depersonalization. They elevate mood and energy levels, but unnecessary use can result in feelings of disconnection from oneself and surroundings.
Cannabis use can induce depersonalization-derealization disorder, especially in high doses or in susceptible individuals. Its psychoactive compounds affect perception and cognition. It can lead to a sense of unreality or disconnection from the self.
Exploring the connection between drug use and DPD sheds light on the complex interplay between substance abuse and mental illness.
Drug-initiated depersonalization stems from a combination of neurological changes and psychological triggers. Here’s the detail of the underlying mechanisms:
Different drugs can affect various neurotransmitters (chemical messengers in the brain) differently. For example, substances like marijuana, psychedelics, or dissociative drugs can impact neurotransmitters like serotonin or glutamate, which are involved in regulating mood and perception. These changes can upset the normal functioning of brain regions responsible for self-awareness and perception, leading to experiences of detachment or unreality.
Psychological factors such as the setting in which the drug is consumed, and the individual’s mental state can all influence the experience. For example, using drugs in unfamiliar or uncomfortable environments or feeling anxious or stressed beforehand can increase the likelihood of experiencing depersonalization.
By knowing these mechanisms, we can better grasp the challenges people face when dealing with drug-induced depersonalization.
Drug-induced depersonalization disorder manifests through a range of symptoms that can be categorized into physical, emotional, and cognitive domains.
Physical symptoms of derealization disorders often manifest as a sense of detachment from one’s own body and unusual sensory experiences. Some common symptoms are:
These physical symptoms can be deeply unsettling, contributing to the overall distress experienced by patients with DPD.
Emotional symptoms of DPD involve a profound sense of dissociation from one’s feelings. Here are some emotional indicators:
These emotional disturbances can significantly impact personal relationships, exacerbating the effects of emotional abuse experienced by individuals.
Cognitive signs of DPD often include disturbing thoughts about reality and challenges with concentration and memory. Common cognitive manifestations are:
These disruptions can interfere with daily functioning and exacerbate the feelings of detachment signs of DPD from drug or alcohol abuse.
Diagnostic criteria for personality disorders involve an integrated approach to ensure accurate identification and differentiation from other similar conditions.
A clinical evaluation is the first step in diagnosing depersonalization disorder. Mental health professionals or doctors will conduct a detailed interview, asking about symptoms, their duration, and their impact on daily life.
Clinical decision support (CDS) provides tools in mental health settings that might aid clinicians in recognizing dissociative symptoms. CDS guides differential diagnosis, suggesting appropriate treatment options based on evidence-based guidelines.
Differential diagnosis involves distinguishing DPD from others with similar symptoms, such as anxiety, depression, or dissociative identity disorder. This process ensures an accurate diagnosis by considering all possible conditions and ruling out those that don’t match the patient’s specific symptoms.
Screening tools and questionnaires are standardized forms that help identify symptoms of psychotic disorder. These tools, like the Cambridge Depersonalization Scale, allow individuals to report their experiences systematically. The results assist clinicians in understanding the severity and nature of the symptoms, aiding in the diagnosis process.
Through careful evaluation, differential diagnosis, and screening tools, clinicians or doctors can accurately diagnose DPD.
Depersonalization disorder can be challenging, but several treatment options are accessible to help manage its symptoms and improve quality of life. Some main treatment approaches are:
Psychotherapy is a key treatment for DPD, aiming to help persons understand and manage their symptoms. Cognitive behavioral therapy (CBT) focuses on changing negative thought patterns and behavioral events. Mindfulness practices or talk therapy teach individuals to prevent perceptions of detachment and unreality of surroundings.
Other therapeutic interventions like dialectical behavior therapy (DBT) can also be valuable. DBT focuses on building skills in emotion regulation, distress tolerance, and interpersonal effectiveness, which are often areas of difficulty for individuals with DPD.
Medications can also help manage symptoms of depersonalization disorder. Antidepressants, like SSRIs, may reduce anxiety and depression associated with DPD. Antipsychotics are sometimes prescribed to address severe symptoms, though their effectiveness varies. Pharmacotherapy often complements psychotherapy for a comprehensive approach to treatment response.
Therapeutic interventions like repetitive transcranial magnetic stimulation (rTMS) offer a promising adjunctive treatment option for DPD. By targeting specific areas of the brain implicated in DPD symptoms, rTMS aims to modulate neural activity and alleviate distress. Research suggests that rTMS may help regulate abnormal brain functioning associated with DPD.
Adopting healthy lifestyle changes can support DPD treatment. Daily exercise, a balanced diet, and proper sleep improve mental wellness. Self-care practices like mindfulness exercises, relaxation techniques, and stress management can reduce symptoms. Building a strong support network with friends and family also plays a vital role in recovery.
By combining different interventions, individuals with substance use disorder (SUD) can achieve better symptom management.
A proactive approach to preventing drug-induced DPD involves raising awareness about the risks and equipping individuals with healthy coping skills.
Educating people about the risk factors of drug use is vital. Education includes explaining how certain substances can alter brain chemistry and lead to mental health conditions like depersonalization. Awareness programs can help individuals make informed decisions and avoid harmful substances.
Implementing safe practices and harm reduction strategies can minimize the risks of traumatic events associated with drug use. It includes promoting the use of less harmful alternatives and offering support for individuals to reduce their drug abuse. Such measures can significantly lower the chances of experiencing drug-induced depersonalization.
Teaching effective coping mechanisms for stress and anxiety can help prevent attacks of chronic depersonalization. Techniques such as mindfulness, regular exercise, and seeking social support can enhance mental resilience. By managing stress and anxiety healthily, individuals can reduce their vulnerability to mental health disorders.
Through a combination of informed choices and robust coping mechanisms, the likelihood of symptoms from drug and alcohol addiction increases.
Certain recreational drugs like cannabis, hallucinogens (like LSD or magic mushrooms), ketamine, and prescription medications used for anxiety or depression can cause depersonalization. Illicit drug use can change the way your brain works, leading to feelings of detachment from yourself or reality.
Depersonalization can be scary and unsettling, making you feel like you’re outside of your body or disconnected from your emotions. It’s important to be cautious with any substance you put into your body and to seek help if you’re experiencing distressing symptoms like depersonalization.
The drug-induced depersonalization can go away, but it depends on various factors like the type of drug, dosage, individual differences, and whether the drug use stops. In many cases, when the drug wears off or is no longer used, depersonalization gradually fades away.
However, it might take time for the brain and body to readjust, and some people might need the help of medical professionals via therapy or medication to recover fully. It’s essential to seek support if experiencing depersonalization after drug use to get medical help and guidance for recovery.
If you’re experiencing depersonalization and you’ve been using drugs, it’s essential to consider if the symptoms started or got worse after drug use. Depersonalization can be a side effect of some drugs, especially hallucinogens like LSD or certain types of marijuana.
You notice a strong connection between using drugs and feeling disconnected from yourself or reality, and drug use is likely contributing to your symptoms. Keep track of when the symptoms occur and if they improve when you stop using drugs. It’s essential to talk to healthcare professionals who can provide support and guidance tailored to your situation.
Are you or someone dear to you battling substance-induced mental health issues and seeking a treatment program? Let The Recovery Team-Newton guide you through the path to recovery.
Our day treatment program offers flexible support and therapy sessions outside residential settings. It allows people to maintain their daily routines while receiving medical care. Our dual diagnosis services address mental health disorders and substance abuse by providing integrated treatment strategies.
Mental wellness is central to overall well-being and quality of life. Call (508) 978-2772 for support on mental health recovery.

The Recovery Team-Newton explores whether taking Lyrica with Suboxone is safe. Explore potential risks and guidelines

Learn about Suboxone injection side effects and explore recovery solutions in this guide by The Recovery Team-Newton.